Unfortunately, adults quite often neglect hand washing, guided by various considerations: fear of accelerated skin aging from constant contact with water and degreasers (mainly women), lack of comfortable conditions for carrying out such a procedure under certain working conditions, or simply not giving of great importance this procedure. Following the rule alone - “wash your hands before eating and after using the toilet” is not enough and it is recommended to wash your hands much more often.
This issue is particularly acute at catering establishments, trade enterprises and in child care institutions. To employees of such institutions particularly stringent requirements are imposed, because The health of hundreds of people depends on how scrupulously they follow the rules of hand hygiene. But even those who cannot be accused of not following these rules do not always do it correctly.
We remind you of the main points that are recommended to be followed when carrying out the hand washing procedure.
- Personnel involved in food production are required to wash and, if necessary, disinfect their hands: before any food handling, immediately after using the toilet or blowing their nose, and after handling potentially contaminated material.
- Fingernails should be clean and trimmed.
- Hygiene of food production personnel also includes the organization of a sanitary gateway - a system consisting of shoe cleaning, hand washing and disinfection units.
- Washstands should be equipped with liquid soap, skin sanitizer, disposable paper towels, a pedal-operated waste bin, and handwashing instructions.
- Skin hand sanitizers should be readily available at all stages of the work process.
Hand hygiene algorithm:
- Point one. Remove jewelry from your hands (rings, bracelets that go below the wrist, etc.).
- Point two. Turn on the tap, wash your hands with soap.
- Point three . Lather your hands again (both inner and outer outside, between your fingers), wash the soap off your hands.
- Point four. Dry with an electric towel or dry your hands, preferably with a disposable towel.
- If necessary, apply a skin antiseptic to dry hands in accordance with the instructions for use.
It is important to know:
- - simply wet hands that have not been washed thoroughly are a wonderful environment for the proliferation of microbes, so - do not skimp on soap and do not be lazy to foam it well on the skin of your hands; - the more foaming it produces, the more effective soap is when treating skin;
- - the towel or hand wipes must be clean and dry. They should be changed as often as possible.
The rules are simple, but for some reason few people strive to follow them with special care, and yet the effectiveness of the procedure directly depends on how well the hands were soaped or how thoroughly they were wiped at the end of the procedure.
In toilet rooms, bactericidal agent is poured into dispensers. liquid soap.
This increases protective measures, destroys pathogenic microorganisms, fungi, and prevents the occurrence of epidemics. Sprays with disinfectants are effectively used to treat the hands of workers serving food or waiters working in conditions of limited free time.
The leaflet was prepared by L.S. Goncharova, an employee of the Civil Defense and Veterinary Institution Department of the Federal Budgetary Institution of Health “Center for Hygiene and Epidemiology in the Kaliningrad Region”.
Indications for hand hygiene:
Before direct contact with the patient
Before putting on sterile gloves and after removing gloves when placing a central intravascular catheter;
Before and after placement of central intravascular, peripheral vascular and urinary catheters or other invasive devices, if these manipulations do not require surgical intervention;
After contact with the patient's intact skin (for example, when measuring pulse or blood pressure, repositioning the patient, etc.);
After contact with body secretions or excreta, mucous membranes, dressings;
When performing various manipulations to care for a patient after contact with areas of the body contaminated with microorganisms;
After contact with medical equipment and other objects located in close proximity to the patient.
Hand hygiene technique:
With this type of treatment, the use of a skin antiseptic is mandatory. To disinfect hands, use alcohol-containing and other approved skin antiseptics. Antiseptics are used, including gels in individual packaging (small-volume bottles), which are disposed of after use.
When choosing skin antiseptics, detergents and hand skin care products, one should take into account their skin tolerance, the intensity of skin coloring, the presence of fragrance, etc.
Hygienic treatment of the hands with the skin is carried out by rubbing it into the skin of the hands in the amount recommended by the instructions for use, paying special attention to the treatment of the fingertips, the skin around the nails, between the fingers. An indispensable condition for effective hand disinfection is maintaining them in wet within the recommended processing time. When using most alcohol-containing skin antiseptics, pour 2.5 - 5 ml of the drug onto the palms and rub it into the skin of the hands for 2.5 - 3 minutes, repeating the hand washing technique until they are completely dry.
Medical personnel must be provided in sufficient numbers effective means for washing and disinfecting hands, as well as hand skin care products (creams, lotions, balms, etc.) to reduce the risk of contact dermatitis associated with washing and disinfecting them.
Surgical treatment of hands.
Indications for surgical treatment of hands:
Before any surgical or equivalent interventions;
Before the delivery.
Technique for surgical hand antisepsis:
Before treating surgeons' hands, remove watches, bracelets, rings, and signet rings.
Processing is carried out in two stages:
Stage I - washing hands with soap and water for two minutes, and then drying with a sterile towel (napkin), hands are washed with soap in accordance with the hand washing technique, grabbing the skin of the forearms (to the elbow) and observing the direction of washing - from fingers to elbow;
Stage II - treatment of hands, wrists and forearms with a skin antiseptic.
The amount of skin antiseptic required for treatment, the frequency of treatment and its duration are determined in the guidelines/instructions for use of a particular product. An indispensable condition for effective disinfection of hands is keeping them moist for the recommended treatment time, then not wiping the hands until they are completely dry.
Sterile gloves are put on immediately after the skin antiseptic has completely dried.
The use of gloves in health care facilities serves 3 purposes:
Gloves reduce the risk of occupational infection of personnel when in contact with patients and their biological material;
Gloves reduce the risk of contamination of personnel’s hands with transient microbes and transmission to patients;
Gloves reduce the risk of infecting patients with microbes resident on the hands of medical personnel.
Gloves must be worn in all cases where contact with blood or other biological substrates, potentially or obviously contaminated with microorganisms, mucous membranes, or damaged skin is possible.
It is not allowed to use the same pair of gloves when in contact (for care) with two or more patients, when moving from one patient to another, or from a body area contaminated with microorganisms to a clean one. After removing gloves, perform hand hygiene.
When gloves become contaminated with secretions, blood, etc. To avoid contamination of your hands during the process of removing them, you should use a swab (napkin) moistened with a solution of a disinfectant (or antiseptic) to remove visible dirt. Remove gloves, immerse them in the product solution, then discard. Treat your hands with an antiseptic.
Use of sterile gloves:
To perform any surgical interventions and similar manipulations;
When carrying out dressings;
When working with intravenous catheters;
When performing lumbar punctures;
When placing a urinary catheter;
During intubation;
When working with any wound surfaces;
During vaginal examination;
When carrying out any endoscopic examinations and medical procedures;
When working with sterile material and drugs;
When working with immunocompromised patients.
Use of disinfected gloves (or clean gloves if the gloves are disposable):
In clinical diagnostic laboratories, bacteriological laboratories, when working with any biological material (blood, urine, cerebrospinal fluid, etc.);
When performing intramuscular, subcutaneous, intradermal, intravenous and cutaneous injections;
When performing any disinfection work;
When working with cytostatics and other chemicals;
In prosthesis when working with any material.
Treatment of reusable gloves after use is carried out according to the same scheme as reusable instruments: disinfection - pre-sterilization cleaning - sterilization. To sterilize gloves, it is advisable to use soft packages in small packages (no more than 10 pairs). With this packaging, sterilization of gloves is easier than in bags. Before sterilization, gloves are soaped, lined with gauze or paper on the inside, then unfolded and folded in pairs, placing a layer of gauze between the gloves. Each pair is wrapped in gauze or a napkin. The gloves come unfolded in the package. Sterilization is carried out in an autoclave at 120C – 1.1 atm – 45 minutes.
Places for sanitizing the hands of medical personnel must be equipped in accordance with the requirements of SanPiN 2.1.3.2630-10. In case of violation of the requirements of the specified SanPiN, the Code of Administrative Offenses provides for a number of penalties. For example, for a person who violates these requirements, a fine from 1,000 rubles to 2,000 rubles, and for a medical organization - from 10,000 rubles to 20,000 rubles or temporary cessation of activities. Below we will look at how to organize the process of cleaning the hands of employees.
Hand treatment of medical personnel according to SanPiN
For high-quality processing According to SanPin, medical personnel must ensure that each room is equipped with a washbasin connected to the water supply. Required condition- Availability hot water and taps with mixer.
“Correct and timely disinfection of the hands of medical staff, without a doubt, is the key to the safety of both the employees of medical institutions and patients. There is such a thing as infections associated with the provision of medical care(HAI). And reducing the risk of their occurrence can be considered one of the priorities in the work of a clinic of any profile. According to the World Health Organization, out of 100 hospitalized patients, at least 7 are infected with HAIs.
HCAIs are often associated with the treatment of hands by medical staff of the clinic, because they become the source of pathogenic microorganisms for the patient. Nowadays, hand washing by medical personnel or treating them with skin antiseptics are extremely relevant infection control measures. Moreover, one must understand that pathogenic microorganisms often appear not only on the surface of infected wounds, but also on areas of absolutely healthy skin.
In the Russian Federation, the rules for treating the hands of medical employees are defined by SanPiN 2.1.3.2630-10 “Sanitary and epidemiological requirements for organizations engaged in medical activities.” Hand treatment is performed depending on the nature of the medical procedure being performed. Among the mandatory requirements are the employee’s nails being cut short, without chemical (varnish) coating, and no jewelry.
There are two types of disinfection of the hands of medical workers: hygienic hand treatment and disinfection of the hands of surgeons. Naturally, in the second case the processing is of a deeper nature. As for hygienic treatment, it is always required - before any contact with the patient. In particular, it involves washing hands with soap, as well as treating them with a skin antiseptic. To wash your hands, use liquid soap, dispensed using a dispenser, but without too hot water. At the same time, alcohol-based skin antiseptics are considered more effective compared to water-based antiseptics. Before operations, the surgeon’s hands are treated in both ways, and washing in water should last at least two minutes.
The third way to protect the hands of medical staff, as well as prevent HAIs, is medical gloves - this is perhaps one of the most “protected” ways of interacting with patients."
In areas equipped for treating the hands of medical personnel, in addition to washbasins, there should be special devices for use when washing hands with liquid soap and antiseptics. It is necessary to ensure that they always have means for washing and disinfecting hands. In addition, hand care products should also be nearby. Near the washbasin it is necessary to install a bucket that can be opened using a foot drive. There should also be paper towels there.
Dispensers for applying liquid soap and antiseptics should be installed not only near washbasins, but also in other areas accessible to employees. For example, clause 12.4.6 ch. I SanPiN 2.1.3.2630–10 indicates that dispensers can be installed at the entrance to wards, in the corridors and locks of departments, at the beds of intensive care and seriously ill patients, on work and manipulation tables.
You might be interested:
Hand washing of medical personnel according to SanPiN: how to choose a dispenser
To treat the hands of medical personnel in accordance with SanPiN, clinics have a dispenser - this is a special device for dispensing something in a certain quantity. These devices should be selected based on your needs. For example, a dispenser can be either a mechanical push dispenser or a wall-mounted one with an elbow drive (with replaceable pumps) and even a touch dispenser that operates without contact. In addition, systems that automatically dispense liquid soap or antiseptic are also considered dispensers.
EXPERT SPEAKS
Dmitry Gornastolev, chief physician of the Medscan network of medical centers
“The global benchmark for patient safety is the JCI standards, specifically the International Patient Safety Goals (IPSG).
In the Russian Federation, hand sanitization of medical personnel is regulated by SanPiN 2.1.3.2630-10. The nature of the medical procedure performed requires a certain level of reduction in microbial contamination of the skin. Hygienic or surgical treatment of the hands of medical staff is carried out.
Hand hygiene – medical personnel must sanitize their hands during the working day and when performing medical procedures.
Surgical treatment of hands - is carried out in cases where the patient undergoes manipulations that are accompanied by damage to the skin (invasive manipulations) or surgical methods treatment, incl. performing a biopsy under the control of computed tomography. This hand treatment differs from the hygienic one in terms of the time required and the technology of the process. Surgical debridement is more thorough and requires a higher degree of skin disinfection to further reduce patient contamination.
The processing agents are usually the same. And alcohol-based products show greater effectiveness.
In case of an emergency, hand hygiene allows you to simply treat your hands with an antiseptic and put on sterile gloves. Surgical treatment of hands in routine practice does not allow this. Such processing is permissible only in military field conditions (and extremely difficult situations, when every second counts).
Surgical hand treatment begins with the use of soap and has its own characteristics:
- hand treatment begins with the fingertips and ends with the forearm;
- must take at least 5 minutes;
- The dorsum of the hands, interdigital spaces, nail beds, palms, wrist and forearm should be treated;
- after treating the hands (from the tips to the forearm), the hands are washed again, but only the wrist part, the forearm is not processed again;
- Next comes double treatment with an antiseptic (in the same sequence as when washing with soap);
- After exposure of the skin to the antiseptic, sterile gloves are put on and medical procedures are performed.
Proper hand cleaning by medical personnel significantly reduces the incidence of infectious complications, reduces the consumption of antibiotics and reduces the cost of hospital care."
Before purchasing a dispenser for repeated use, you should review the manufacturer's information to ensure that the manufacturer specifies how to clean the dispenser. If the dispenser is intended to be filled with an alcohol-containing antiseptic, then a permit is required for its use with flammable materials.
The advantage is that the dispenser operates without contact and has a set of disposable cartridges. The device must have accurate, indelible markings with the liquid level, as well as an area for placing a label with the name of the antiseptic used. The instructions for the dispenser must contain information that it can be used with liquids from various manufacturers and that the dispenser can be machine cleaned and disinfected.
Before refilling the dispenser, be sure to clean and disinfect the container. If the dispenser is partially filled, then you should not add a new dose of liquid soap or antiseptic.
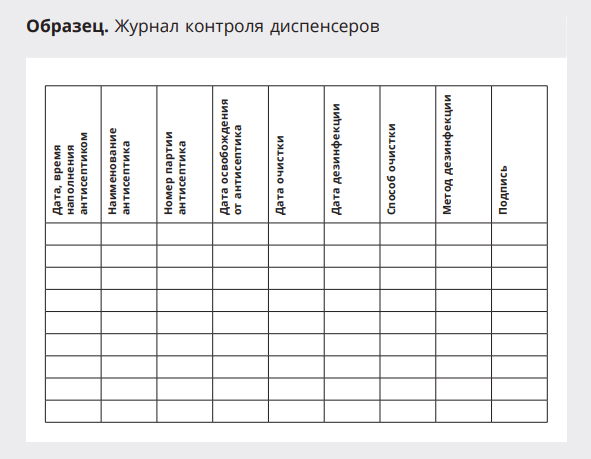
In order to control the dispenser maintenance procedure, it is worth keeping a log - a sample below.
Hand sanitizing of medical personnel is a simple but effective method of preventing the development of hospital-acquired infections.
In the article we will tell you what type of processing and algorithm to use in accordance with the requirements of SanPiN.
In addition, this is a guarantee of health safety for both patients and medical workers.
↯ More articles in the magazine
From the article you will learn
Types of processing
Exist different levels and methods of disinfection (see table), but not all experts appreciate these techniques, and are often limited to simple rinsing.
Open a new SOP by medical treatment hands from the experts of the Chief Nurse System. For each type, a clear and clear algorithm was identified.
|
What is it used for? |
When is it carried out? |
|
|
Using water and soap |
1. Removal of visible contaminants. 2. Removing dangerous bacteria |
|
|
Using antiseptic |
Destruction of any potentially dangerous microorganisms |
|
|
Surgical |
Aimed at getting rid of visible contaminants and destroying dangerous bacteria, as well as reducing the number of dangerous microflora. |
|
Hygienic treatment of the hands of medical staff: algorithm
The goal with this method is to remove any visible contaminants, as well as transient microflora.
This is necessary in order to exclude the possibility of transferring such microflora to other healthcare workers and patients.
3 requirements for hygienic hand washing according to SanPin:
- Before starting, the doctor must remove jewelry and watches - under them accumulation big number microbes;
- The specialist’s nails should be cut short, and it is undesirable to have varnish on them.
- The sleeves of the medical gown must be rolled up 2/3 so that they do not interfere.
SanPiN requirements require careful soaping. After this they are washed with running water warm water, and the procedure is repeated.
This is due to the fact that with a single wash, dirt and harmful microorganisms are removed only from the skin of the hands. When the doctor rinses the soap with warm water, the pores open, allowing any remaining germs to be removed.
The hand treatment of medical personnel is shown in the diagram below.

Calculator: calculation of antiseptic for treating the hands of the dressing team
Use the online calculator to calculate the need for alcohol-containing antiseptics for cleaning the hands of members of the dressing team, for bandaging and disinfecting wounds. The calculator was developed by specialists from the Chief Nurse System.
Surgical treatment: algorithm
This is a routine, mandatory procedure before any interventions are performed on patients.
The entire process consists of a number of steps, as well as several techniques and skills that allow you to achieve effective and high-quality cleaning.
Processing is carried out in a specially designated place. It should have a sink with a mixer with hot and cold water.
Scheme for hand treatment of medical personnel


Purpose of hand debridement
Main and fundamental goal surgical treatment– remove dangerous microflora from the doctor’s skin that can be transferred to the patient during surgery.
Processing stages

At the first stage, the doctor should thoroughly wash the area of the hands and forearms with soap.
To do this, use warm tap water, under which the skin is washed with regular soap for 2-3 minutes. When the doctor is finished, he should use a sterile wipe to dry the skin.
At the second stage the skin is treated with a special antiseptic.
An alcohol-based antiseptic is applied to the dry skin of the wrists, forearms and hands. It is important to use enough product throughout the application to keep the skin moist until the end of the procedure.
When the steps are completed, the doctor puts on sterile gloves and can begin the operation.
Standard “Handwashing at a social level”
Target: removal of dirt and transient flora from contaminating skin on the hands of medical personnel resulting from contact with patients or objects environment; ensuring infectious safety of patients and staff.
Indications: before distributing food, feeding the patient; after visiting the toilet; before and after caring for the patient, unless hands are contaminated with the patient's body fluids.
Prepare: liquid soap in dispensers for single use; clock with second hand, paper towels.
Action algorithm:
1. Remove rings, rings, watches and other jewelry from your fingers, check the integrity of the skin of your hands.
2. Fold the sleeves of the robe over 2/3 of your forearms.
3. Open water tap using a paper napkin and adjust the water temperature (35°-40°C), thereby preventing hand contact with microorganisms located on the tap.
4.
Wash your hands with soap and water running water up to 2/3 of the forearm for 30 seconds, paying attention to the phalanges, interdigital spaces of the hands, then wash the back and palm of each hand and rotate the base thumbs hands (this time is enough for decontamination of hands at a social level, if the surface of the skin of the hands is washed thoroughly and no dirty areas of the skin of the hands are left).
5. Rinse your hands under running water to remove soap suds (hold your hands with your fingers up so that the water flows into the sink from your elbows, without touching the sink. The phalanges of your fingers should remain the cleanest).
6. Close the elbow valve using your elbow.
7. Dry your hands with a paper towel; if you don't have an elbow tap, seal the edges with a paper towel.
Standard “Hand hygiene at a hygienic level”
Target:
Indications: before and after performing invasive procedures; before putting on and after removing gloves, after contact with body fluids and after possible microbial contamination; before caring for an immunocompromised patient.
Prepare: liquid soap in dispensers; 70% ethanol, watch with second hand, warm water, paper towel, safe disposal container (SCU).
Action algorithm:
1. Remove rings, rings, watches and other jewelry from your fingers.
2. Check the integrity of the skin on your hands.
3. Fold the sleeves of the robe over 2/3 of your forearms.
4. Open the water tap using a paper napkin and adjust the water temperature (35°-40°C), thereby preventing hand contact with microorganisms. located on the tap.
5. Lather your hands vigorously under a moderate stream of warm water until
2/3 forearms and wash your hands in the following sequence:
- palm on palm;
Each movement is repeated at least 5 times within 10 seconds.
6. Rinse your hands under warm running water until the soap is completely removed, holding your hands so that your wrists and hands are above elbow level (in this position, the water flows from the clean area to the dirty area).
7. Close the tap with your right or left elbow.
8. Dry your hands with a paper towel.
If there is no elbow valve, close the valve using a paper towel.
Note:
- Without necessary conditions for hygienic hand washing, you can treat them with an antiseptic;
- apply to dry hands 3-5
ml of antiseptic and rub it onto the skin of your hands until dry. Do not wipe your hands after treatment! It is also important to observe the exposure time - hands must be wet from the antiseptic for at least 15 seconds;
- the principle of surface treatment “from clean to dirty” is observed. Do not touch foreign objects with washed hands.
1.3. Standard “Hygienic treatment of hands with antiseptic”
Target: removal or destruction of transient microflora, ensuring infectious safety of the patient and staff.
Indications: before injection, catheterization. operation
Contraindications: presence of pustules on the hands and body, cracks and wounds of the skin, skin diseases.
Prepare; skin antiseptic for treating the hands of medical personnel
Action algorithm:
1. Carry out hand decontamination at a hygienic level (see standard).
2. Dry your hands with a paper towel.
3. Apply 3-5 ml of antiseptic to your palms and rub it into the skin for 30 seconds in the following sequence:
- palm on palm
- right palm on the back of the left hand and vice versa;
- palm to palm, fingers of one hand in the interdigital spaces of the other;
- the backs of the fingers of the right hand across the palm of the left hand and vice versa;
- rotational friction of the thumbs;
- with the fingertips of the left hand brought together right palm circular movements and vice versa.
4. Ensure that the antiseptic on the skin of your hands dries completely.
Note: before you start using a new antiseptic, you need to study guidelines to him.
1.4. Standard “Wearing Sterile Gloves”
Target: ensuring infectious safety of patients and staff.
- gloves reduce the risk of occupational infection when in contact with patients or their secretions;
- gloves reduce the risk of contamination of personnel’s hands with transient pathogens and their subsequent transmission to patients,
- gloves reduce the risk of infection of patients with microbes that are part of the resident flora of the hands of medical workers.
Indications: when performing invasive procedures, in contact with any biological fluid, in violation of the integrity of the skin of both the patient and the medical worker, during endoscopic examinations and manipulations; in clinical diagnostic, bacteriological laboratories when working with material from patients, when performing injections, when caring for the patient.
Prepare: gloves in sterile packaging, safe disposal container (KBU).
Action algorithm:
1. Decontaminate your hands at a hygienic level and treat your hands with an antiseptic.
2. Take gloves in sterile packaging and unwrap them.
3. Grasp the right-hand glove by the lapel with your left hand so that your fingers do not touch inner surface glove lapel.
4. Close the fingers of your right hand and insert them into the glove.
5. Open the fingers of your right hand and pull the glove over them without disturbing its cuff.
6. Place the 2nd, 3rd and 4th fingers of the right hand, already wearing the glove, under the lapel of the left glove so that the 1st finger of the right hand is directed towards the 1st finger on the left glove.
7. Hold the left glove vertically with the 2nd, 3rd and 4th fingers of the right hand.
8. Close the fingers of your left hand and insert them into the glove.
9. Open the fingers of your left hand and pull the glove over them without disturbing its cuff.
10. Straighten the lapel of the left glove, pulling it over the sleeve, then on the right using the 2nd and 3rd fingers, bringing them under the folded edge of the glove.
Note: If one glove is damaged, you must immediately change both, because you cannot remove one glove without contaminating the other.
1.5. Standard "Removal of gloves"
Action algorithm:
1. Using the gloved fingers of your right hand, make a flap on the left glove, touching only the outside of it.
2. Using the gloved fingers of your left hand, make a flap on the right glove, touching it only from the outside.
3. Remove the glove from your left hand, turning it inside out.
4. Hold the glove removed from your left hand by the lapel in your right hand.
5.
With your left hand, grab the glove on your right hand by the lapel with inside.
6. Remove the glove from your right hand, turning it inside out.
7. Place both gloves (the left one inside the right one) in the KBU.
Composition of the cleaning solution
3. Immerse disassembled medical devices completely in the cleaning solution for 15 minutes, after filling the cavities and channels with the solution, and close the lid.
4. Use a brush (gauze swab) to soak each item in the washing solution for 0.5 minutes (pass the washing solution through the channels).
5.
Place medical supplies in the tray.
6. Rinse each product under running water for 10 minutes, passing water through the channels and cavities of the products.
7. Carry out quality control of pre-sterilization cleaning with an azopyram sample. 1% of simultaneously processed products of the same type per day, but not less than 3-5 units, are subject to control.
8. Prepare a working solution of the azopyram reagent (the working reagent can be used for 2 hours after preparation).
9. Apply the working reagent with a “reagent” pipette to medical products (on the body, channels and cavities, places of contact with biological fluids).
10. Hold medical devices over cotton wool or tissue, observing the color of the reagent flowing off.
11. Evaluate the result of the azopyram test.
Standard "Ear Care"
Target: maintaining the patient’s personal hygiene, preventing diseases, preventing hearing loss due to the accumulation of sulfur, instilling a medicinal substance.
Indications: patient’s serious condition, presence of wax in the ear canal.
Contraindications: inflammatory processes in the auricle, external auditory canal.
Prepare: sterile: tray, pipette, tweezers, beaker, cotton pads, napkins, gloves, 3% hydrogen peroxide solution, soap solution, containers with disinfectant solutions, KBU.
Action algorithm:
1. Explain the procedure to the patient and obtain his consent.
3. Prepare a container with soap solutions.
4. Tilt the patient’s head in the direction opposite to the ear being treated and place the tray.
5. Moisten a cloth in a warm soapy solution and wipe the auricle, dry with a dry cloth (to remove dirt).
6. Pour a 3% solution of hydrogen peroxide, preheated in a water bath (T 0 – 36 0 – 37 0 C), into a sterile beaker.
7. Take a cotton turunda with tweezers in your right hand and moisten it with a 3% hydrogen peroxide solution, and with your left hand pull the auricle back and top to align the ear canal and insert the turunda with rotational movements into the external auditory canal to a depth of no more than 1 cm for 2 - 3 minutes.
8. Insert the dry turunda with light rotational movements into the external auditory canal to a depth of no more than 1 cm and leave for 2 - 3 minutes.
9. Remove the turunda with rotational movements from the external auditory canal - this ensures the removal of secretions and wax from the ear canal.
10. Treat the other ear canal in the same sequence.
11. Remove gloves.
12. Place used gloves, turundas, napkins in the KBU, tweezers, beaker in containers with disinfectant solutions.
13. Wash and dry your hands.
Note: when treating ears, cotton wool should not be wound onto hard objects, as injury to the ear canal may occur.
Action algorithm:
1. Explain to the patient the purpose of the procedure and obtain his consent.
2. Decontaminate your hands at a hygienic level and wear gloves.
3. Place an oilcloth under the patient.
4. Pour warm water into the basin.
5. Expose the patient's upper body.
6. Soak a napkin, part of a towel or a cloth mitten in warm water, and lightly squeeze out excess water.
7. Wipe the patient’s skin in the following sequence: face, chin, behind the ears, neck, arms, chest, folds under the mammary glands, armpits.
8. Dry the patient’s body with the dry end of the towel in the same sequence and cover with a sheet.
9. Treat the back, thighs, legs in the same way.
10. Trim your fingernails.
11. Change underwear and bed linen (if necessary).
12. Remove gloves.
13. Wash and dry your hands.
Action algorithm:
1. Wash the hair of a seriously ill patient in bed.
2. Give your head an elevated position, i.e. place a special headrest or roll up the mattress and tuck it under the patient’s head, lay an oilcloth on it.
3. Tilt the patient's head back at neck level.
4. Place a bowl of warm water on a stool at the head of the bed at the level of the patient's neck.
5.
Wet the patient's head with a stream of water, lather the hair, and thoroughly massage the scalp.
6. Wash your hair from the frontal part of the head back with soap or shampoo.
7. Rinse your hair and wring it dry with a towel.
8. Comb your hair with a fine-toothed comb daily, short hair should be combed from roots to ends, and long hair should be divided into strands and combed slowly from ends to roots, being careful not to pull them out.
9. Place a clean cotton scarf on your head.
10. Lower the headrest, remove all care items, and straighten the mattress.
11. Place used care items in disinfectant solution.
Note:
- seriously ill patients should wash their hair (in the absence of contraindications) once a week. The optimal device for this procedure is a special headrest, but the bed should also have a removable backrest, which greatly facilitates this labor-intensive procedure;
- women comb their hair daily with a fine comb;
- men have their hair cut short;
- a fine-tooth comb dipped in a 6% vinegar solution is good for combing out dandruff and dust.
Standard "Vessel supply"
Target: providing physiological functions to the patient.
Indication: used by patients on strict bed rest and bed rest for bowel movements and Bladder. Prepare: disinfected vessel, oilcloth, diaper, gloves, diaper, water, toilet paper, container with disinfectant solution, KBU.
Action algorithm:
1. Explain to the patient the purpose and course of the procedure, obtain his consent,
2. Rinse the vessel with warm water, leaving some water in it.
3. Separate the patient from others with a screen, remove or fold back the blanket to the lower back, place an oilcloth under the patient’s pelvis and a diaper on top.
4. Decontaminate your hands at a hygienic level and wear gloves.
5. Help the patient turn on his side, legs slightly bent at the knees and spread at the hips.
6. Place your left hand under the sacrum on the side, helping the patient lift the pelvis.
7. With your right hand, move the diaper under the patient’s buttocks so that his perineum is above the opening of the vessel, while moving the diaper towards the lower back.
8. Cover the patient with a blanket or sheet and leave him alone.
9. At the end of the bowel movement, turn the patient slightly to one side while holding the bedpan right hand, remove it from under the patient.
10. Wipe the anal area toilet paper. Place the paper in the vessel. If necessary, wash the patient and dry the perineum.
11.Remove the bedpan, oilcloth, diaper and screen. Replace the sheet if necessary.
12.
Help the patient lie down comfortably, cover with a blanket .
13.
Cover the vessel with a diaper or oilcloth and take it to toilet room.
14.
Pour the contents of the vessel into the toilet, rinse it with hot water .
15.
Immerse the vessel in a container with disinfectant solution, discard gloves in
KBU.
16.
Wash and dry your hands.
Excreted liquid
9. Record the amount of fluid you drink and inject into your body on a record sheet.
Injected liquid
10. At 6:00 am next day The patient gives the record sheet to the nurse.
The difference between the amount of fluid you drink and the daily amount at night is the amount of water balance in the body.
The nurse should:
- Ensure that the patient can perform a fluid count.
- Ensure that the patient has not taken diuretics within 3 days before the study.
- Tell the patient how much fluid should be excreted in the urine normally.
- Explain to the patient the approximate percentage of water in food to facilitate accounting for the administered fluid (not only the water content in the food is taken into account, but also the administered parenteral solutions).
- Solid foods can contain between 60 and 80% water.
- Not only urine, but also vomit and feces of the patient are taken into account.
- The nurse calculates the amount of input and output per night.
The percentage of fluid excreted is determined (80% of the normal amount of fluid excreted).
amount of urine excreted x 100
Excretion percentage =
amount of fluid administered
Calculate water balance using the following formula:
multiply the total amount of urine excreted per day by 0.8 (80%) = the amount of night that should be excreted normally.
Compare the amount of fluid released with the amount of normal fluid calculated.
- Water balance is considered negative if less fluid is released than calculated.
- The water balance is considered positive if more fluid is released than calculated.
- Make entries on the water balance sheet and evaluate it.
Result evaluation:
80% - 5-10% - excretion rate (-10-15% - in the hot season; +10-15%
- in cold weather;
- positive water balance (>90%) indicates the effectiveness of treatment and resolution of edema (reaction to diuretics or fasting diets);
- negative water balance (10%) indicates an increase in edema or ineffectiveness of the dose of diuretics.
I.IX. Punctures.
1.84. Standard "Patient Preparation and medical instruments to perform pleural puncture (thoracentesis, thoracentesis)."
Target: diagnostic: study of the nature of the pleural cavity; therapeutic: introduction of drugs into the cavity.
Indications: traumatic hemothorax, pneumothorax, spontaneous valve pneumothorax, respiratory diseases (lobar pneumonia, pleurisy, pulmonary empyema, tuberculosis, lung cancer, etc.).
Contraindications: increased bleeding, skin diseases (pyoderma, herpes zoster, chest burns, acute heart failure.
Prepare: sterile: cotton balls, gauze pads, diapers, needles for intravenous and subcutaneous injections, puncture needles 10 cm long and 1 - 1.5 mm in diameter, syringes 5, 10, 20, 50 ml, tweezers, 0. 5% novocaine solution, 5% alcohol solution of iodine, 70% alcohol, clamp; cleol, adhesive plaster, 2 chest x-rays, sterile container for pleural fluid, container with disinfectant solution, referral to the laboratory, kit for assistance with anaphylactic shock, gloves, CBU.
Action algorithm:
2. Place the patient, undressed to the waist, on a chair facing the back of the chair, ask him to lean on the back of the chair with one hand and place the other (from the side of the pathological process) behind his head.
3. Ask the patient to slightly tilt their torso in the direction opposite to where the doctor will perform the puncture.
4. Only a doctor performs a pleural puncture; a nurse assists him.
5. Decontaminate your hands at a hygienic level, treat them with a skin antiseptic, and put on gloves.
6. Treat the intended puncture site with a 5% alcohol solution of iodine, then with a 70% alcohol solution and again with iodine.
7. Give the doctor a syringe with a 0.5% solution of novocaine for infiltration anesthesia of the intercostal muscles and pleura.
8. The puncture is made in the VII - VII intercostal spaces along the upper edge of the underlying rib, since the neurovascular bundle passes along the lower edge of the rib and intercostal vessels can be damaged.
9. The doctor inserts a puncture needle into the pleural cavity and pumps out the contents into a syringe.
10. Place a container for the liquid to be removed.
11. Release the contents of the syringe into a sterile jar (test tube) for laboratory testing.
12. Give the doctor a syringe with a filled antibiotic for injection into the pleural cavity.
13. After removing the needle, treat the puncture site with a 5% alcohol solution of iodine.
14. Apply a sterile napkin to the puncture site and secure with adhesive tape or cleol.
15. Tightly bandage the chest with sheets to slow down the exudation of fluid into the pleural cavity and prevent the development of collapse.
16. Remove gloves, wash hands and dry.
17. Place used disposable syringes, gloves, cotton balls, napkins in the KBU, puncture needle in a container with disinfectant solution.
18. Monitor the patient’s well-being, the condition of the bandage, count his pulse, measure his blood pressure.
19. Escort the patient to the room on a gurney, lying on his stomach.
20. Warn the patient about the need to remain in bed for 2 hours after the procedure.
21. Send what you receive biological material for research in the laboratory with a referral.
Note:
When more than 1 liter of fluid is removed from the pleural cavity at a time, there is a high risk of collapse;
Delivery of pleural fluid to the laboratory must be carried out immediately to avoid the destruction of enzymes and cellular elements;
When a needle enters the pleural cavity, a feeling of “falling” into the free space appears.
1.85. Standard "Preparation of the patient and medical equipment for abdominal puncture (laparocentesis)."
Target: diagnostic: laboratory examination of ascitic fluid.
Therapeutic: removal of accumulated fluid from the abdominal cavity during ascites.
Indications: ascites, with malignant neoplasms of the abdominal cavity, chronic hepatitis and cirrhosis of the liver, chronic cardiovascular failure.
Contraindications: severe hypotension, adhesions in the abdominal cavity, severe flatulence.
Prepare: sterile: cotton balls, gloves, trocar, scalpel, syringes 5, 10, 20 ml, napkins, jar with lid; 0.5% novocaine solution, 5% iodine solution, 70% alcohol, container for extracted liquid, basin, test tubes; a wide towel or sheet, an adhesive plaster, a kit to help with anaphylactic shock, a container with a disinfectant solution, a referral for examination, dressing material, tweezers, KBU.
Action algorithm:
1. Inform the patient about the upcoming study and obtain his consent.
2. On the morning of the test, give the patient a cleansing enema until the effect of “pure water” is achieved.
3. Immediately before the procedure, ask the patient to empty his bladder.
4. Ask the patient to sit in a chair, leaning on its back. Cover the patient's legs with oilcloth.
5. Decontaminate your hands at a hygienic level, treat them with a skin antiseptic, and put on gloves.
6. Give the doctor a 5% alcohol solution of iodine, then a 70% alcohol solution to treat the skin between the navel and pubis.
7. Give the doctor a syringe with a 0.5% solution of novocaine to carry out layer-by-layer infiltration anesthesia of soft tissues. A puncture during laparocentesis is made according to midline anterior abdominal wall at an equal distance between the navel and pubis, stepping back 2-3 cm to the side.
8. The doctor incises the skin with a scalpel, pushes the trocar through the thickness of the abdominal wall with a drilling motion with his right hand, then removes the stylet and ascitic fluid begins to flow through the cannula under pressure.
9. Place a container (basin or bucket) in front of the patient for fluid flowing from the abdominal cavity.
10. Take 20 - 50 ml of liquid for laboratory testing (bacteriological and cytological) into a sterile jar.
11. Place a sterile sheet or wide towel under the patient’s lower abdomen, the ends of which should be held by the nurse. Cover the abdomen with a sheet or towel covering it above or below the puncture site.
12. Using a wide towel or sheet, periodically tighten the patient's anterior abdominal wall as fluid is removed.
13. After completing the procedure, you need to remove the cannula, close the wound with a skin suture and treat it with a 5% iodine solution, apply an aseptic bandage.
14. Remove gloves, wash hands and dry.
15. Place the used instruments in a disinfectant solution, place gloves, cotton balls, and syringes in the KBU.
16. Determine the patient’s pulse and measure blood pressure.
17. Transport the patient to the room on a gurney.
18. Warn the patient to remain in bed for 2 hours after the procedure (to avoid hemodynamic disorders).
19. Send the obtained biological material for testing to the laboratory.
Note:
When performing manipulations, strictly follow the rules of asepsis;
With rapid fluid withdrawal, collapse and fainting may develop due to a drop in intra-abdominal and intrathoracic pressure and redistribution of circulating blood.
1.86. Standard "Preparation of the patient and medical instruments for performing a spinal puncture (lumbar)".
Target: diagnostic (for studying cerebrospinal fluid) and therapeutic (for administering antibiotics, etc.).
Indications: meningitis.
Prepare: sterile: syringes with needles (5 ml, 10 ml, 20 ml), puncture needle with mandrel, tweezers, napkins and cotton balls, tray, nutrient medium, test tubes, gloves; manometric tube, 70% alcohol, 5% alcohol solution of iodine, 0.5% novocaine solution, adhesive plaster, KBU.
Action algorithm:
1. Inform the patient about the upcoming procedure and obtain consent.
2. The puncture is performed by a doctor under conditions of strict adherence to aseptic rules.
3. Take the patient to the treatment room.
4. Lay the patient on his right side closer to the edge of the couch without a pillow, tilt his head forward to his chest, bend his legs as much as possible at the knees and pull them towards the stomach (the back should arch).
5. Push it in left hand under the patient's side, hold the patient's legs with your right hand to fix the position given to the back. During the puncture, another assistant fixes the patient's head.
6. The puncture is made between the III and IV lumbar vertebrae.
8. Treat the skin at the puncture site with a 5% iodine solution, then with a 70% alcohol solution.
9. Fill a syringe with a 0.5% solution of novocaine and give it to the doctor for infiltration anesthesia of soft tissues, and then a puncture needle with a mandrel on the tray.
10. Collect 10 ml of cerebrospinal fluid in a tube, write the directions and send to the clinical laboratory.
11. Collect 2-5 ml of cerebrospinal fluid into a test tube with nutrient medium for bacteriological examination. Write a referral and send the biological material to the bacteriological laboratory.
12. Give the doctor a manometric tube to determine the cerebrospinal fluid pressure.
13. After removing the puncture needle, treat the puncture site with a 5% alcohol solution of iodine.
14. Place a sterile napkin over the puncture site and cover with adhesive tape.
15. Place the patient on his stomach and take him on a gurney to the ward.
16. Place the patient on the bed without a pillow in the prone position for 2 hours.
17. Observe the patient’s condition throughout the day.
18. Remove gloves.
19. Place syringes, cotton balls, gloves in the KBU, place the used instruments in a disinfectant solution.
20. Wash and dry.
1.87. Standard "Preparation of the patient and medical equipment for sterile puncture."
Target: diagnostic: examination of bone marrow to establish or confirm the diagnosis of blood diseases.
Indications: diseases of the hematopoietic system.
Contraindications: myocardial infarction, attacks of bronchial asthma, extensive burns, skin diseases, thrombocytopenia.
Prepare: sterile: tray, syringes 10 - 20 ml, Kassirsky puncture needle, glass slides 8 - 10 pieces, cotton and gauze balls, forceps, tweezers, gloves, 70% alcohol, 5% alcohol solution of iodine; adhesive plaster, sterile dressing material, KBU.
Action algorithm:
1. Inform the patient about the upcoming study and obtain his consent.
2. Sternal puncture is performed by a doctor in the treatment room.
3. The sternum is punctured at the level of the III - IV intercostal space.
4. The nurse assists the doctor during the procedure.
5. Invite the patient into the treatment room.
6. Invite the patient to undress to the waist. Help him lie down on the couch, on his back without a pillow.
7. Decontaminate your hands at a hygienic level, treat them with a skin antiseptic, and put on gloves.
8. Treat the front surface of the patient’s chest, from the collarbone to the gastric region, with a sterile cotton ball moistened with a 5% iodine solution, and then 2 times with 70% alcohol.
9. Perform layer-by-layer infiltration anesthesia of soft tissues with a 2% novocaine solution up to 2 ml in the center of the sternum at the level of III - IV intercostal spaces.
10. Give the doctor a Kassirsky puncture needle, installing a limiter shield at 13 - 15 mm of the needle tip, then a sterile syringe.
11. The doctor pierces the outer plate of the sternum. The hand feels the failure of the needle; after removing the mandrin, a 20.0 ml syringe is attached to the needle and 0.5 - 1 ml of bone marrow is sucked into it, which is poured onto a glass slide.
12. Dry the slides.
13. After removing the needle, treat the puncture site with a 5% alcohol solution of iodine or a 70% alcohol solution and apply a sterile bandage and secure with an adhesive plaster.
14. Remove gloves.
15. Dispose of used gloves, syringes and cotton balls in the CBU.
16. Wash your hands with soap and dry.
17. Show the patient to the room.
18. Send the slides to the laboratory after the material has dried.
Note: Kassirsky's needle is a short, thick-walled needle with a mandrin and a shield that protects against too much deep penetration needles.
1.88. Standard "Preparation of the patient and medical instruments for joint puncture."
Target: diagnostic: determining the nature of the contents of the joint; therapeutic: removing effusion, washing the joint cavity, introducing medicinal substances into the joint.
Indications: joint diseases, intra-articular fractures, hemoarthrosis.
Contraindications: purulent inflammation of the skin at the puncture site.
Prepare: sterile: puncture needle 7 - 10 cm long, syringes 10, 20 ml, tweezers, gauze swabs; aseptic dressing, napkins, gloves, tray, 5% alcohol solution of iodine, 70% alcohol solution, 0.5% novocaine solution, test tubes, KBU.
Action algorithm:
1. The puncture is performed by a doctor in a treatment room under conditions of strict adherence to aseptic rules.
2. Inform the patient about the upcoming study and obtain his consent.
3. Decontaminate your hands at a hygienic level, treat them with a skin antiseptic, and put on gloves.
4. Ask the patient to sit comfortably in a chair or assume a comfortable position.
5. Give the doctor a 5% alcohol solution of iodine, then a 70% alcohol solution to treat the intended puncture site, and a syringe with a 0.5% novocaine solution for infiltration anesthesia.
6. The doctor covers the joint at the puncture site with his left hand and squeezes the effusion to the puncture site.
7. The needle is inserted into the joint and the effusion is collected with a syringe.
8. Pour the first portion of the contents from the syringe into the test tube without touching the walls of the test tube for laboratory testing.
9. After puncture, antibiotics and steroid hormones are injected into the joint cavity.
10. After removing the needle, lubricate the puncture site with a 5% alcohol solution of iodine and apply an aseptic bandage.
11. Place used syringes, napkins, gloves, gauze swabs in the KBU, puncture needle in the disinfectant solution.
12. Remove gloves, wash and dry your hands.
I.XII. “Preparation of the patient for laboratory and instrumental research methods.”
Standard “Preparation of the patient for fibrogastroduodenoscopy”
Target: provide quality training to research; visual inspection mucous membrane of the esophagus, stomach and duodenum
Prepare: sterile gastroscope, towel; referral for research.
FGDS is performed by a doctor and a nurse assists.
Action algorithm:
1. Explain to the patient the purpose and course of the upcoming study and obtain his consent.
2. Swipe psychological preparation patient.
3. Inform the patient that the study is carried out in the morning on an empty stomach. Eliminate food, water, medicines; do not smoke, do not brush your teeth.
4. Provide the patient with a light dinner the night before no later than 6 p.m.; after dinner, the patient should not eat or drink.
5.
Make sure that the patient removes removable dentures before the examination.
6. Warn the patient that during endoscopy he should not speak or swallow saliva (the patient spits saliva into a towel or napkin).
7. Take the patient to the endoscopy room with a towel, medical history, and directions to the appointed time.
8. Escort the patient to the room after the study and ask him not to eat for 1-1.5 hours until swallowing is completely restored; no smoking.
Note:
-
SC remedication is not carried out, because changes the condition of the organ being studied;
- when taking material for a biopsy, food is served to the patient only cold.
Standard “Preparation of the patient for colonoscopy”
Colonoscopy - This is an instrumental method for examining high-lying parts of the colon using a flexible endoscope probe.
Diagnostic value of the method: Colonoscopy allows you to directly